Introduction:In situ vaccination aims to induce an immune response locally at one tumor site, that propagates systemically to all tumor sites. Prior clinical studies have demonstrated that this strategy can be effective in indolent lymphoma (Brody et al., JCO 2010, Frank et al., Cancer Discov 2018, Hammerich et al., Nat Med 2019). The underlying mechanisms, however, remain unclear, as immune recognition and destruction of cancer cells occurs at the level of the tumor microenvironment (TME), and the human TME has been difficult to study due to challenges in acquiring adequate tissue samples. Here, we directly investigate changes induced in the TME by in situ vaccination, applying single cell methods to serial samples from patients on a clinical trial, and relate these changes to clinical tumor response.
Methods: We profiled serial specimens from 2 sites of disease in 10 indolent lymphoma patients enrolled in an in situ vaccination trial (NCT02927964). Motivated by compelling preclinical data demonstrating the efficacy of intratumoral CpG, a TLR9 agonist, and systemic ibrutinib, a BTK inhibitor (Sagiv-Barfi et al., Blood 2015), patients receive local low-dose radiation and CpG intratumorally to one site of disease and begin oral ibrutinib in the second week of treatment. Tumor fine needle aspirates (FNAs) from the injected and a distant uninjected tumor site as well as peripheral blood samples are obtained prior to, and at 1 and 6 weeks after treatment start. Single cells from the FNAs and blood samples are then subject to droplet-based single cell RNA sequencing, with approximately 3,000-10,000 cells sequenced per sample.
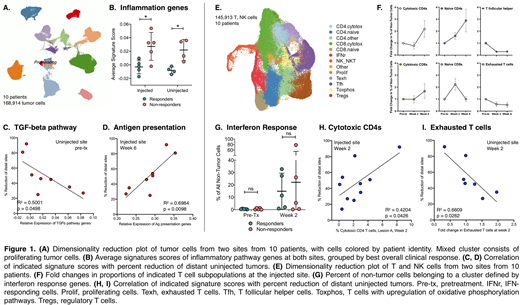
Results: In total, we analyzed 314,827 cells from 52 tumor samples and 30 peripheral blood samples (Fig. 1A). At both the local injected and the distant uninjected tumor sites, we found significant changes in proportions and transcriptional phenotypes of tumor and immune cells, several of which tracked with clinical response. Upon treatment, the proportions of tumor cells decreased significantly at the treated site, even within the 6-week time frame (p=0.003). Increased expression of inflammation related genes at both the injected and uninjected sites (Fig. 1B) and of TGFb pathway genes at the uninjected site (Fig. 1C) were negatively associated with clinical response. Conversely, high expression of antigen presentation genes by week 6 at the injected site correlated with greater shrinkage of distant uninjected tumors (Fig. 1D). Among T and NK cells (Fig. 1E), we observed treatment-induced increases in naïve and cytotoxic CD4 and CD8 T cells, and reductions in T follicular helper and exhausted T cells (Fig. 1F). While all patients exhibited strong interferon responses in their T and NK cells, the degree of interferon response was not associated with overall clinical response (Fig. 1G). Instead, higher cytotoxic CD4 T cells at the injected site and fewer exhausted T cells at the uninjected site after treatment correlated with clinical response.
Conclusions: By sampling multiple tumors over time in patients undergoing in situ vaccination, we identify significant changes in tumor and microenvironmental cells at both the injected and uninjected sites, several of which associate with clinical tumor regression. Our approach represents successful application of single-cell genomics to a clinical trial, illuminating treatment-induced cellular dynamics, and implicating tumor cell antigen presentation and CD4 T cell responses as possible determinants of clinical response.
Levy:Immunocore: Membership on an entity's Board of Directors or advisory committees; Walking Fish: Membership on an entity's Board of Directors or advisory committees; Viracta: Membership on an entity's Board of Directors or advisory committees; Quadriga: Membership on an entity's Board of Directors or advisory committees; Beigene: Membership on an entity's Board of Directors or advisory committees; GigaGen: Membership on an entity's Board of Directors or advisory committees; Teneobio: Membership on an entity's Board of Directors or advisory committees; Sutro: Membership on an entity's Board of Directors or advisory committees; Checkmate: Membership on an entity's Board of Directors or advisory committees; Nurix: Membership on an entity's Board of Directors or advisory committees; Dragonfly: Membership on an entity's Board of Directors or advisory committees; Abpro: Membership on an entity's Board of Directors or advisory committees; Apexigen: Membership on an entity's Board of Directors or advisory committees; Spotlight: Membership on an entity's Board of Directors or advisory committees; 47 Inc.: Membership on an entity's Board of Directors or advisory committees; XCella: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal